
Glaucoma Services
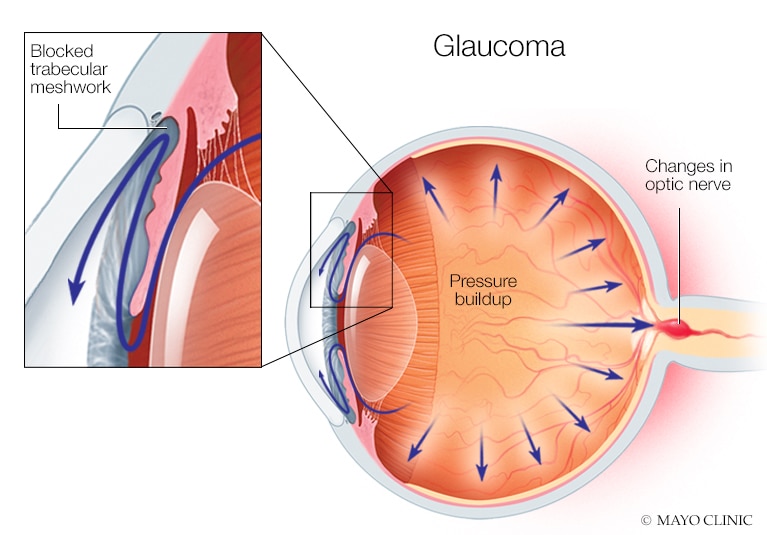
Glaucoma is a group of conditions that all lead to progressive optic nerve damage (neuropathy). This nerve damage affects the visual system by damaging and ultimately killing the retinal ganglion cells that transmit visual information from the retina to the brain. Although glaucoma may not be considered solely as an “eye disease,” the bottom line is damage to or degeneration of the optic nerve.
Glaucoma is characterized by:
- a specific pattern of optic nerve head damage called “cupping”
- an identifiable pattern of visual field loss
A variety of risk factors may contribute to the structural (nerve damage) and functional (vision loss) damage associated with glaucoma, high intraocular pressure being a significant factor in glaucomatous nerve damage. Glaucoma can result in vision loss and blindness. However, with early detection and treatment, you can often protect your eyes against serious vision loss.
Because of the range of disorders involved, it’s important that you understand the criteria your doctor uses for a glaucoma diagnosis.
Can glaucoma develop if my eye pressure is high?
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher levels of eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important. It can help your eye care professional determine what level of eye pressure is normal for you.
Can glaucoma develop without an increase in my eye pressure?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is a type of open-angle glaucoma.
Who is at risk for open-angle glaucoma?
A comprehensive dilated eye exam can reveal more risk factors, such as high eye pressure, thinness of the cornea, and abnormal optic nerve anatomy. In some people with certain combinations of these high-risk factors, medicines in the form of eye drops reduce the risk of developing glaucoma by about half.
Anyone can develop glaucoma.
Some people, listed below, are at higher risk than others:
- Indians over age 40
- Everyone over age 60
- People with a family history of glaucoma
Diagnosing Glaucoma
Because it often goes undetected in its early stages, glaucoma is so silent when it develops that there are many currently have glaucoma are unaware of their condition.
Glaucoma Symptoms
Open-angle glaucoma usually has no symptoms. There is no pain. Vision stays normal. Glaucoma can develop in one or both eyes.
Left untreated, people with glaucoma slowly lose their peripheral (side) vision. As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. They seem to be looking through a tunnel. Over time, straight-ahead (central) vision may decrease until no vision remains.
Normal Vision The same scene as viewed by a person with glaucoma
How is glaucoma detected?
Glaucoma is detected through a comprehensive dilated eye exam that includes the following:
Visual acuity test. This eye chart test measures how well you see at various distances.
Visual field test. This test measures your peripheral (side vision). It helps your eye care professional tell if you have lost peripheral vision, a sign of glaucoma.
Dilated eye exam. In this exam, drops are placed in your eyes to widen, or dilate, the pupils. The eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
Tonometry is the measurement of pressure inside the eye by using an instrument called a tonometer. Numbing drops may be applied to your eye for this test. A tonometer measures pressure inside the eye to detect glaucoma.
Pachymetry is the measurement of the thickness of your cornea. Sunayan’s eye care professional applies a numbing drop to your eye and uses an ultrasonic wave instrument to measure the thickness of your cornea.
Can glaucoma be cured?
No. There is no cure for glaucoma.
Vision lost from the disease cannot be restored.
Glaucoma Treatments
Immediate treatment for early-stage, open-angle glaucoma can delay progression of the disease. That’s why early diagnosis is very important.
Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma.
Medicines
Medicines, in the form of eye drops or pills, are the most common early treatment for glaucoma. Taken regularly, these eyedrops lower eye pressure. Some medicines cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye.
Before you begin glaucoma treatment, tell our eye care professional about other medicines and supplements that you are taking. Sometimes the drops can interfere with the way other medicines work.
Glaucoma medicines need to be taken regularly as directed by our eye care professional. Most people have no problems. However, some medicines can cause headaches or other side effects. For example, drops may cause stinging, burning, and redness in the eyes.
Many medicines are available to treat glaucoma. If you have problems with one medicine, kindly inform our eye care professional. Treatment with a different dose or a new medicine may be possible.
Because glaucoma often has no symptoms, people may be tempted to stop taking, or may forget to take, their medicine. You need to use the drops or pills as they help control your eye pressure. Regular use is very important.
A tonometer measures pressure inside the eye to detect glaucoma.
Our eye care professionals show you how to put the drops into your eye.
Follow-up visits are essential to check your eye pressure and monitor progress.
If you have glaucoma in both eyes, usually only one eye will be treated at a time. Laser treatments for each eye will be scheduled several days to several weeks apart.
Studies show that laser surgery can be very good at reducing the pressure in some patients. However, its effects can wear off over time. Your doctor may suggest further treatment.
Conventional surgery
Conventional surgery makes a new opening for the fluid to leave the eye. Your doctor may suggest this treatment at any time. Conventional surgery often is done after medicines and laser surgery have failed to control pressure.
Conventional surgery, called trabeculectomy, is performed in an operating room. Before the surgery, you are given medicine to help you relax. Your doctor makes small injections around the eye to numb it. A small piece of tissue is removed to create a new channel for the fluid to drain from the eye. This fluid will drain between the eye tissue layers and create a blister-like “filtration bleb.”
For several weeks after the surgery, you must put drops in the eye to fight infection and inflammation. These drops will be different from those you may have been using before surgery.
Conventional surgery is performed on one eye at a time. Usually the operations are four to six weeks apart.
Conventional surgery is about 60 to 80 percent effective at lowering eye pressure. If the new drainage opening narrows, a second operation may be needed. Conventional surgery works best if you have not had previous eye surgery, such as a cataract operation.
Sometimes after conventional surgery, your vision may not be as good as it was before conventional surgery. Conventional surgery can cause side effects, including cataract, problems with the cornea, inflammation, infection inside the eye, or low eye pressure problems. If you have any of these problems, tell your doctor so a treatment plan can be developed.
Questions for Your Doctor
- Which glaucoma tests should I have?
- What do these tests involve?
- Do you have the equipment needed to perform these tests? If not, where will the tests be carried out?
- Will the tests hurt?
- How often should I be tested for glaucoma?
- How long will it take to learn the results?
What do I need to do to in order to find out the test results?
Test Results and Diagnosis
Glaucoma is usually diagnosed when examination and/or testing shows one or both of the following:
- Structural changes: characteristic optic nerve head and the retinal nerve fiber layer degeneration.
- Loss of functional vision: defects in visual fields that match the structural changes.
Your examination results will indicate one of three possibilities:
- You do not have glaucoma and are not currently at risk for developing glaucoma.
- You do not appear to have glaucoma, but you have risk factors that indicate that further examination by an ophthalmologist is in order, or that you should return for periodic re-examinations.
- You have glaucoma.
Glaucoma Tests
There is no single test for determining whether you have glaucoma or are at risk of developing glaucoma. The clinician examining you must interpret your medical history (including any earlier examination findings), family history (genetics), and results from clinical observation of your optic nerve head and diagnostic test(s), and then assess if 1) there are structural changes and/or loss of functional vision that require treatment, or 2) if you are at risk of such damage and should begin treatment to manage potential disease.
To detect glaucoma, you should have a comprehensive dilated eye examination with an emphasis on these assessments:
Do you Have Glaucoma?
Your Test Results
Your test results should answer these questions for you and the doctor making a diagnosis:
- Optic nerve: Do you have visible optic nerve rim and/or nerve fibre layer damage?
- Visual fields: Do you have visual field defects or scotomas that follow a glaucomatous pattern?
- Pressure: Is your IOP normal or above normal?
- Angle: Are your angles open, narrow, or closed?
- Risk factors: How many risk factors do you have?
- Corneal thickness: What is your corneal thickness measurement?
Diagnosis
If you do not have any observable optic nerve damage and do not have elevated IOP or several risk factors, you may be considered free of glaucoma and not in need of ongoing observation.
Something to keep in mind is that with glaucoma, observable functional loss often follows structural loss. Although criteria for diagnosing glaucoma usually include observable and measurable structural and functional damage, optic disc and retinal nerve fiber layer structural changes are often observed before visual field defects are picked up by standard perimetry.
Not only do structural changes appear to precede functional changes, but it is now possible with digital imaging to detect structural retinal nerve fiber layer damage before functional visual field impairment can be measured.
Being a Glaucoma Suspect
Often the results of testing are not clear-cut. Suspicious signs of glaucoma often precede identifiable glaucoma, and if you are a “glaucoma suspect” our eye specialist may suggest early treatment.
Making the Decision on Treatment as a Glaucoma Suspect
Note to readers: This section is not intended to provide medical or treatment advice, nor is it intended to recommend a given course of treatment. Treatment decisions should only be made after consultation with your doctors.
If you are identified as a glaucoma suspect, your doctor will discuss with you whether to begin treatment to minimize the risk of glaucoma developing.
Why not wait until a more definitive diagnosis is possible? Glaucoma develops slowly and its early development often doesn’t show up in examination. By the time glaucoma is apparent to an examiner, the disease has usually been active for some time and the damage done is not reversible.
Evaluating Risk
Whether to wait or to begin treatment ultimately comes down to evaluating as best as one can the risk of not beginning treatment, which is something your doctor can help you determine.
The Right Decision is an Informed Decision
By being well informed about the tests and studies described by our qualified ophthalmologists, you can feel confident that your doctor’s advice is based on the information that is needed to assess your actual risk. With that information you can best decide how to proceed.
Ask and Understand
If you are not offered a chance to discuss your diagnosis and treatment plan, ask to do so. These are decisions that can have life-long implications. Our team is trained to make you aware of your needs to discuss your vision, your prognosis, and decisions about treatment.
Questions for Your Doctor
If you have been identified as a glaucoma suspect, make sure you first understand your test results. You might also ask the following questions:
- How high a risk do you think I have? What is that assessment based on?
- How often will we be monitoring my eyes?
- What will we be monitoring? IOP? Visual fields?
If you have been identified as having glaucoma or a high enough risk to begin treatment, you might ask:
- What is my specific condition?
- What is the prognosis for keeping my sight?
- What treatment options are available?
- What treatment option(s) do you recommend and why?
- What are the pros and cons of your recommended treatment versus alternative treatments?
- How might the treatment help me? What kind of improvements might I expect and how long will it take before we know if the treatment is effective?
- Are there possible side effects?
- How often will we be monitoring my eyes?
- Could my condition and my current functional vision affect my daily life, such as my ability to drive?
Final Thoughts on Diagnosis
Unfortunately, currently there is no single, definitive test for glaucoma. In order to make a diagnostic decision, our doctors evaluate many factors in order to decide if you have glaucoma or are a glaucoma suspect. The more you understand glaucoma, the more empowered you will be to take an active role in the diagnosis.
Take Notes
Glaucoma appointments are stressful. They happen quickly, and most patients are nervous. Dealing with a disease that can take your vision can be frightening. Amid a rapid stressful appointment, it’s easy to forget the questions you wanted to ask. Write down your questions beforehand.
It’s also easy to forget what was said in such a fast-paced, emotionally charged situation. You may get your questions answered only to find when you get home that you can’t remember what the answers were! Take notes or bring along a friend or partner who can record the session, which will free you to listen attentively.
It’s very easy to forget your doctor’s instructions. Instructions are important—don’t leave them to chance. Write down any instructions your doctor gives you. And if you don’t understand the instructions, don’t just write down what you don’t understand—ask questions until you understand.
Caring for Your Vision is Your Responsibility
In the end, it’s your responsibility to make sure you are in a doctor-patient relationship that works for you. This is not simply a matter of feeling good. Glaucoma is a chronic disease, so you may be with your doctor for many years. Trusting your doctor’s opinion and trusting that your doctor is listening to you will affect whether you do your part in the treatment process.
Consider the following questions.
Overall Vision
- Have you noticed a change in your vision?
- Do you accomplish less than you would like because of your vision?
- Do you have difficulty reading ordinary print such as magazines or books?
- Do you have trouble finding something on a crowded shelf?
- Do you have difficulty reading traffic signs?
- Do you have trouble going down steps, stairs, or curbs in dim light or at night?
- While walking, do you have trouble noticing objects off to the side?
- Do you have difficulty seeing how people react to things you say?
- Do you have difficulty picking out and matching your own clothes?
- Do you avoid visiting with people because of your vision?
- Do you have difficulty recognizing faces, even of friends and family?
- Do you have trouble grocery shopping? Making phone calls? Taking medications?
- Can you write checks and manage other financial tasks?
- Do you have trouble driving at night? If so, what is difficult about it?
Loss of Visual Function
- Are there any blurred or distorted areas in your vision?
- Do you see lights doubled?
- Are you affected by glare outdoors, indoors, or both?
- Do you have difficulty seeing under certain lighting conditions?
- Do you notice difficulty seeing objects in low-contrast situations such as a beige sweater on a white bedspread, or figures in dark clothing by the side of the road at dusk?
- Do you see an object more clearly when you look slightly away from it?
- Do you have difficulty seeing things on the periphery of your visual field?
Restricted Visual Fields
- Do you have difficulty getting around by yourself?
- Do you have difficulty finding objects?
- Do you have difficulty functioning in poor light?
Glaucoma and Vision Loss
Vision loss from glaucoma is commonly presented as a gradual reduction in the peripheral field of vision, described and presented visually as increased tunnel vision:
While narrowing of peripheral or side vision is indeed a primary characteristic of glaucoma, there are other, less frequently discussed ways glaucoma affects vision, including:
- loss of contrast
- defects within the field of vision, such as distortion or blind spots
- sensitivity to glare or light
These questions can help you determine if contrast sensitivity is a problem:
- Do you have trouble driving at night? At dusk?
- Do you have trouble reading text on a computer screen/Mobile?
- Do you have difficulty telling the difference between different denominations of paper money?
- Do you trip on the footpath, steps, and stairs
Need Eye Surgery? Book with us in advance
Our experience of more than 16 years of in providing eye checkup, cataract surgery and other procedures to residents throughout West Bengal, India.
